Question 5#
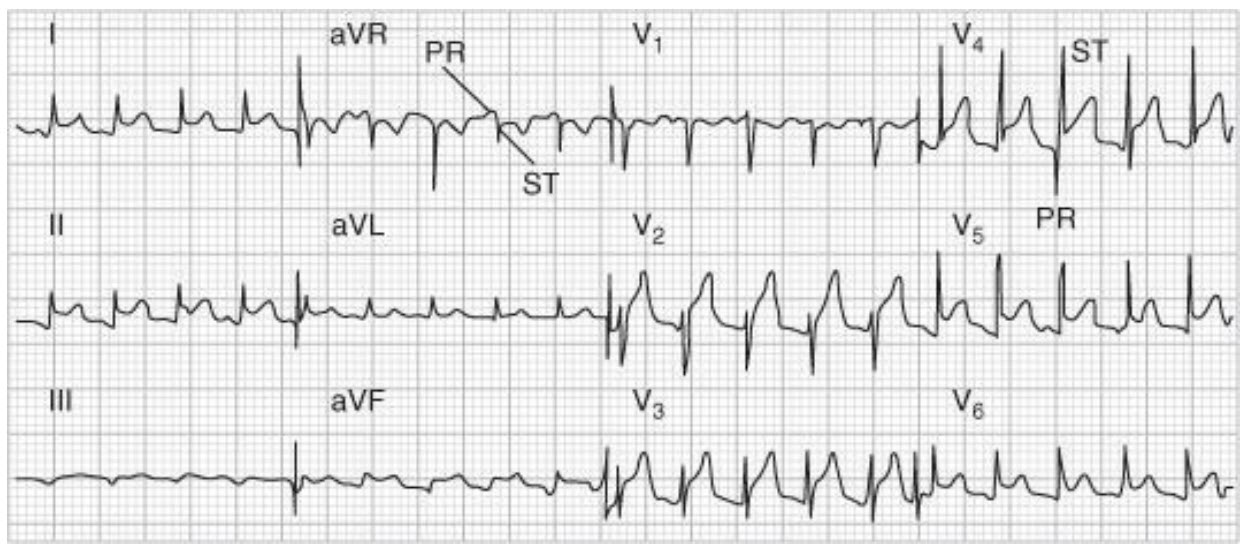
One month after hospital discharge for documented myocardial infarction, a 65-year-old man returns to your office concerned about low-grade fever and chest pain. He describes the chest pain as sharp, worse on deep inspiration and better when sitting up. He denies shortness of breath; his lungs are clear to auscultation. On your heart examination you do not appreciate any murmur or rubs. ECG is shown below. Which therapy is most likely to be effective in relieving his chest pain?
B. Warfarin
C. An anti-inflammatory agent
D. Nitrates
E. An anxiolytic
Correct Answer is C
Comment:
The patient has Dressler syndrome (post–myocardial infarction pericarditis), which may occur about 1 to 2 weeks post–myocardial infarction. It is thought to be an autoimmune phenomenon. The patient may have fever, leukocytosis, and pericardial or pleural effusion. The chest pain associated with pericarditis tends to be pleuritic and worse with sitting which places the pericardium closer to the chest wall. A pericardial friction rub is present in about 85% of patients. Typical ECG changes of pericarditis include diffuse ST-segment elevation. The characteristic PR-segment depression (opposite in polarity to the ST segment) due to a concomitant atrial injury current can also be appreciated in this patient. Acute ST elevation seen with myocardial infarction usually presents with regional or localized (as opposed to diffuse) ST elevation depending on the region of infarction (V1 -V4 in anteroseptal infarction; I, aVL, V5 , V6 in lateral infarction; and II, III, AVF in inferior infarction). Treatment of Dressler syndrome is the same as for other forms of pericarditis. A short course of a nonsteroidal anti-inflammatory agent or corticosteroids may help relieve symptoms. Anticoagulation is not a treatment for this condition, but, if needed for other indications, it should be used cautiously, since hemorrhagic pericarditis may result. A patient recently discharged from the hospital warrants suspicion of pneumonia, but this patient does not have other signs and symptoms suggesting pneumonia. Likewise the patient’s symptoms are not suggestive of anginal pain or panic attack, for which nitrates or anxiolytics might be prescribed.