Question 1#
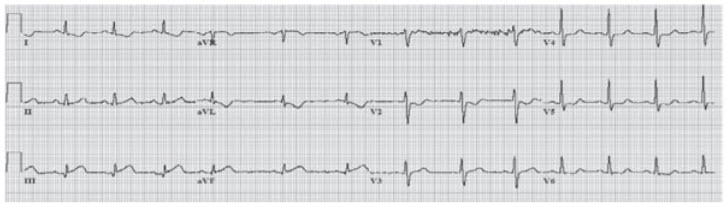
A 68-year-old man presents to the hospital with a 3-hour history of crushing substernal chest pain. He reports that the symptoms developed suddenly and were accompanied by sweating and nausea. The chest pain has been getting worse, is not exacerbated by deep inspiration, and does not radiate to his jaw or either arm. He endorses mild shortness of breath but denies subjective fevers, chills, headache, cough, abdominal pain, and diarrhea. He has a history of coronary artery disease, hypertension, diabetes, and gastroesophageal reflux disease (GERD). He takes aspirin, lisinopril, metformin, and omeprazole. His family history is significant for hypertension in both parents, and his father died of a heart attack at the age of 60. He has a 40 pack-year history of smoking, and denies any alcohol or illicit drug use. On examination, the patient is afebrile with a blood pressure of 150/96 mmHg, heart rate of 89 beats per minute, respiratory rate of 18 breaths per minute, and oxygen saturation of 97% on room air. He appears diaphoretic. There is an S3 on cardiac auscultation, with mildly elevated jugular venous pulsations and bibasilar rales on pulmonary examination. His dorsalis pedis and posterior tibial pulses are diminished bilaterally, with mild swelling around his ankles. His initial laboratory values and ECG (Figure below) are shown below.
- Hemoglobin 14.2 g/dL
- Leukocyte count 9,000/mm3
- Platelets 275,000/mm3
- Sodium 136 mEq/L
- Potassium 4.2 mEq/L
- Chloride 105 mEq/L
- Bicarbonate 22 mEq/L
- Blood urea nitrogen 16 mg/dL
- Creatinine 1.2 mg/dL
- Glucose 145 mg/dL
- Calcium 9.6 mg/dL
- Troponin I Elevated
Which of the following best represents the underlying pathology in this patient?
A. Rupture of a plaque with thrombosis leading to partial occlusion of a coronary arteryB. Vasospasm of a coronary artery
C. Gradual occlusion of a coronary artery by plaque
D. Rupture of a plaque with thrombosis leading to complete occlusion of a coronary artery
E. Superficial erosion of a plaque with thrombosis
Correct Answer is D
Comment:
Rupture of a plaque with thrombosis leading to complete occlusion of a coronary artery. This is an extreme example of a long question that could be answered quickly if the reader first reads what the question is asking. This is a good strategy for long questions, since many students report that time management is challenging for the Medicine shelf examination. In this case, a brief survey of the question and answer choices would reveal that there is a process occurring that involves the patient’s coronary arteries, and therefore all that is necessary is finding the diagnosis (obvious from the ECG) and then picking an answer choice. Much of the long history and examination is unnecessary, which can be skipped or at least skimmed; the laboratory tests are normal with the only significant finding being elevated troponins. The ECG shows ST elevation in the inferior leads (II, III, aVF), confirming the diagnosis of ST elevation myocardial infarction (STEMI). The pathologic process occurring in a STEMI is most commonly due to rupture of an atherosclerotic plaque in the arterial wall of a coronary artery. Rupture of the plaque exposes tissue factor and other thrombogenic subendothelial components, leading to thrombosis and occlusion of the artery. (C) There is usually some degree of gradual narrowing of the artery due to the plaque, but rupture of the plaque with subsequent thrombosis is necessary to produce a STEMI. (A) The coronary artery occlusion is complete (not partial), which causes full thickness myocardial ischemia that manifests with ST elevations on ECG. (B) This answer refers to Prinzmetal angina, which is an unusual cause of myocardial ischemia that typically occurs in women with symptom onset in the evening. (E) Superficial erosion may occur but is not the most common mechanism in acute coronary syndromes (ACS).