Question 21#
A 59-year-old man with a history of coronary artery disease (CAD) and remote coronary bypass surgery presents with progressive dyspnea and vague chest pain. He had a stress echocardiogram for these symptoms that demonstrated normal LV function with no stress-induced wall motion abnormalities. However, he returned to the emergency department a few days later with recurrent symptoms. This time the house officer examining the patient notes 3+ pedal edema. The patient is admitted and started on diuretics. His blood tests are as follows:
- White blood cell count = 11,000
- Hemoglobin = 14.2
- Platelets = 172,000
- Albumin = 4.6
- Urea = 11
- Creatinine = 0.9
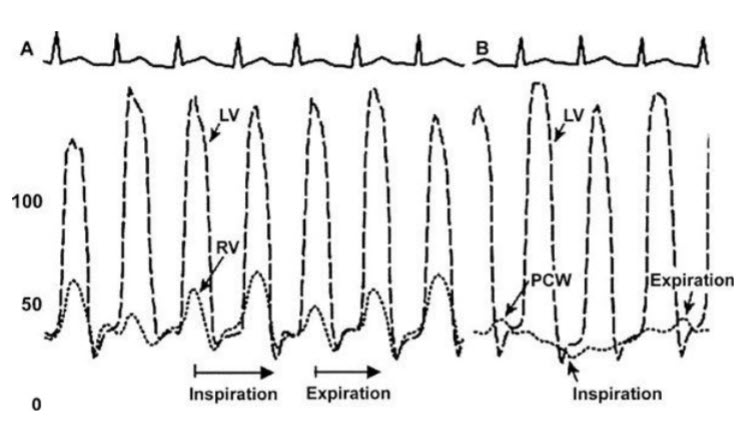
Owing to the recurrent symptoms, his cardiologist decides to refer him for a right and left heart catheterization. The coronary grafts are all patent. The tracings from the study are shown in Figure below.
What is the most logical explanation for this patient’s symptoms?
A. Constrictive pericardial diseaseB. Small-vessel CAD
C. Diastolic dysfunction related to his chronic CAD
D. Cardiac amyloid
E. Cardiac tamponade
Correct Answer is A
Comment:
Constrictive pericardial disease. This patient did not have evidence of ischemia on a recent stress test. Furthermore, there is no evidence of obstructive disease in his coronaries or grafts. His tracings mostly support the diagnosis of constriction, given the diastolic equalization of pressures in the cardiac chambers and the typical square root sign. Amyloidosis would typically show signs of restrictive hemodynamics with no respiratory variation. Echocardiography typically shows increased LV wall thickness. Additionally, a diagnosis of tamponade should have been evident by echocardiography, which the patient had before heart catheterization. Otherwise, hemodynamic tracings of cardiac tamponade would look exactly the same as for constriction.