Question 24#
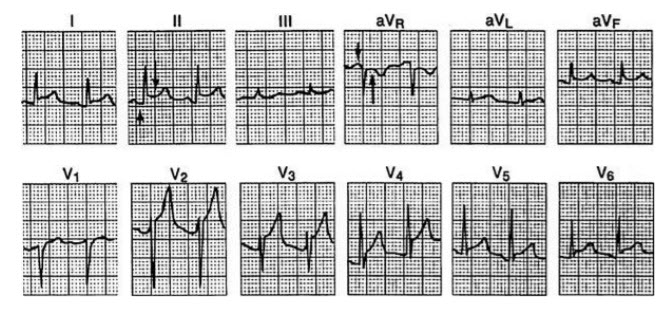
A 58-year-old man, with cardiac risk factors of tobacco use, hypertension, and hypercholesterolemia, presented to the emergency department a few days ago with an acute onset of left-sided chest pain. His evaluation revealed a diaphoretic man in moderate discomfort. An ECG was performed and showed a pattern consistent with an inferior wall acute MI. The patient was treated with thrombolytics. Forty-five minutes after the initial dose of the thrombolytics, he felt better and had complete resolution of his symptoms and normalization of the ECG. On the third day after the event, he reports midsternal chest pain, vague in nature, with mild diaphoresis and shortness of breath. An ECG is performed, as shown in Figure below.
Which of the following should you tell the patient is the next step in managing his condition?
A. There is evidence of reocclusion of the infarct-related artery, and a percutaneous intervention is neededB. There is evidence of reocclusion of the infarct-related artery, and rebolus with thrombolytics and heparin is indicated
C. He is showing signs of early postinfarction pericarditis, and a nonsteroidal anti-inflammatory medication should be started
D. An LV aneurysm has developed, and a TTE is needed to evaluate the extent of the aneurysm
Correct Answer is C
Comment:
He is showing signs of early postinfarction pericarditis, and a nonsteroidal anti-inflammatory medication should be started. This patient had an MI 72 hours ago that was successfully treated with thrombolytics. The ECG shows diffuse ST elevation with PR depression. These findings support the diagnosis of post-MI pericarditis. The ECG changes are new and nonlocalizing. Most patients improve with nonsteroidal anti-inflammatory medications.