Question 7#
A 64-year-old man with hypertension is brought to the emergency department for acute-onset (within the last 60 minutes) left face, arm, and leg weakness. A noncontrast head CT is completed and does not demonstrate a hemorrhage or early ischemic changes. His vitals are BP 174/120, HR 76, and SpO2 99% on room air. A fingerstick blood glucose was obtained and was 127, but other labs are pending.
What is the next BEST step in management for the patient?
A. Administration of tissue plasminogen activator (tPA) at 0.9 mg/kg with initial bolus of 10% total dose and 90% via infusionB. Await coagulation profile (international normalized ratio [INR] and partial thromboplastin time [PTT]) and platelet count before treatment
C. Place a nasogastric tube and Foley catheter followed by administration of tPA
D. Administration of 182 mg rectal aspirin, given patient’s dysarthria
E. Administration of labetolol 10 mg IV push
Correct Answer is E
Comment:
Correct Answer: E
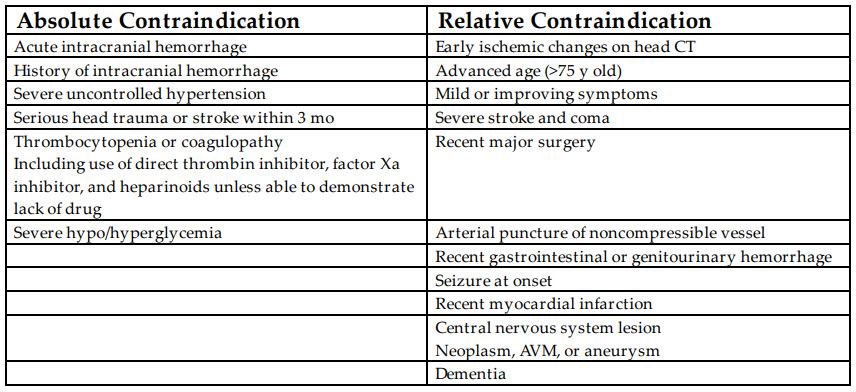
Ischemic stroke is a common neurologic emergency that can result in permanent disability and death. Intravenous tPA has been studied in multiple trials and been found to be effective in acute stroke treatment. The American Heart Association, American Academy of Neurology, and the American Stroke Association have recommendations on the use of tPA in the treatment of ischemic stroke. There are exclusion criteria for treatment with tPA. The initial American tPA study was the NINDS trial, which demonstrated safety (same mortality at 90 days) and efficacy (improved neurologic outcome at 90 days) with use of tPA within 3 hours of neurologic symptoms. ECASS-II and ECASS-III extended the time window from last known well to 4.5 hours. These data demonstrate improved neurologic outcome with treatment in the 3 to 4.5 hour window but further extended to 6 hours with no difference in mortality or outcome. The feared complication of intracerebral hemorrhage can occur with IV tPA treatment. In the case above, the patient has an absolute contraindication to tPA administration, which is BP >185/>110. Treatment of the BP to below this level can then allow for tPA administration, so option E is the right choice.
References:
- Jauch EC, Saver JL, Adams HP Jr, et al. AHA/ASA guideline: guidelines for the early management of patients with acute ischemic stroke. Stroke. 2013;44:870-947.
- Fugate JE, Rabinstein AA. Absolute and relative contraindications to IV rt-PA for acute ischemic stroke. Neurohospitalist. 2015;5:110-121.