Question 7#
A 49-year-old woman requires endotracheal intubation for declining neurologic status. Airway is secured promptly with a rapid sequence induction of ketamine 150 mg and succinylcholine 140 mg. The neurosurgeon on call is on the phone wanting an explanation of why the intracranial pressure (ICP) has elevated to 27 mm Hg.
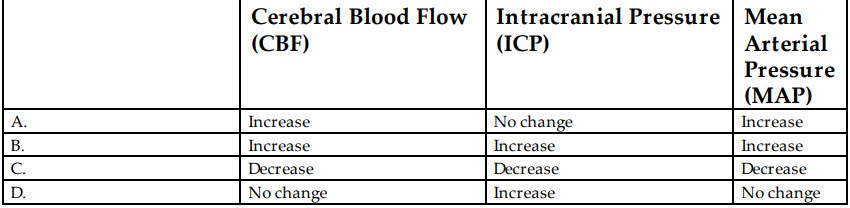
What are the anticipated physiologic effects of ketamine?
B. B
C. C
D. D
Correct Answer is B
Comment:
Correct Answer: B
Ketamine is an NMDA receptor antagonist that provides dissociative effects and can be used to provide rapid anesthesia in intubation scenarios, with dosing typically 1 to 2 mg/kg IV. When used as a sole induction agent, it may increase cerebral blood flow and ICP by virtue of sympathetic stimulation (B). This effect has traditionally warranted the use of other anesthetics in patients with concern for intracranial hypertension. Sympathetic stimulation also preserves or increases mean arterial pressure following induction, provided that the patient’s catecholamine stores are not depleted. Other notable effects include bronchodilation and unpleasant dreams.
References:
- Bucher J, Koyfman A. Intubation of the neurologically injured patient. J Emerg Med. 2015;49:920.
- Himmelseher S, Durieux ME. Revising a dogma: ketamine for patients with neurological injury? Anesth Analg. 2005;101:524.
- Miller M, Kruit N, Heldreich C, et al. Hemodynamic response after rapid sequence induction with ketamine in out-of-hospital patients at risk of shock as defined by the shock index. Ann Emerg Med. 2016;68:181.