Question 9#
A 67-year-old man presents with 3 days of severe substernal chest pain.
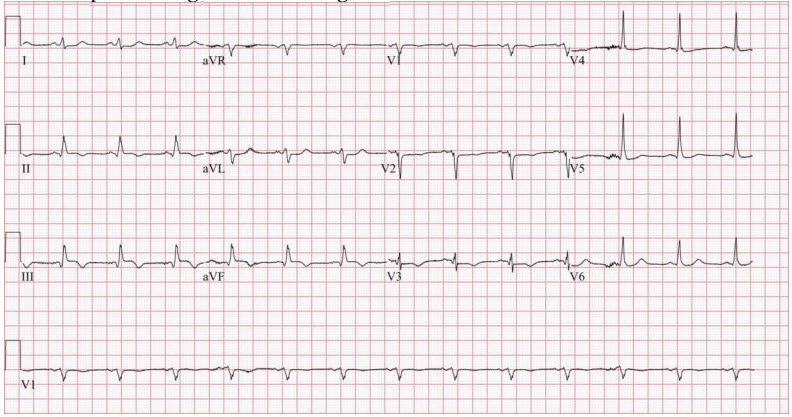
His presenting electrocardiogram is:
A surface echocardiogram reveals an estimated left ventricular ejection fraction of 22% with inferior and inferoseptal akinesis. A 1.5 cm ventricular septal defect at the junction of the inferior wall and septum is noted and is associated with bidirectional shunting. Coronary angiography reveals a 50% narrowing of the ostium of the left main coronary artery, subtotal occlusion of the left anterior descending artery, and total occlusion of the right coronary artery with left to right collaterals. A plan for surgical revascularization, with patch repair of the ventricular septal defect, is formulated. Shortly thereafter, the patient develops progressive cardiogenic shock with ventricular tachycardia.
Which of the following is the next BEST step in management?
A. Insertion of an intra-aortic balloon pump
B. Initiation of inotropic support
C. Percutaneous coronary intervention with drug-eluting stent deployment to the left anterior descending artery
D. Veno-arterial extracorporeal membrane oxygenation (ECMO) initiation
Correct Answer is A
Comment:
Correct Answer: A
Mechanical complications of myocardial infarction include rupture of the ventricular free wall, rupture of the interventricular septum, and rupture of the papillary muscle with acute mitral regurgitation; these can occur within the first 24 hours post–myocardial infarction or as late as 2 weeks. With mainstream revascularization therapies, the incidence of rupture of the interventricular septum occurs in 0.2% of myocardial infarctions. Infarction related to the left anterior descending artery appears to have the highest risk of rupture of the interventricular septum. Definitive management of a post–myocardial infarction ventricular septal rupture necessitates closure. In patients with cardiogenic shock, urgent surgical intervention is necessary. Temporary hemodynamic support can be provided by afterload reduction with vasodilators and intraaortic balloon pump counterpulsation. This minimizes the degree of left to right shunting. Veno-arterial extracorporeal membrane oxygenation (ECMO) could result in a prohibitively high increase in ventricular afterload which would worsen left to right shunting. Inotropes alone may not achieve the goal of afterload reduction.
References:
- Hayashi T, Hirano Y, Takai H, et al. Usefulness of ST-Segment elevation in the inferior leads in predicting ventricular septal rupture in patients with anterior wall acute myocardial infarction. Am J Cardiol. 2005;96(8):1037-1041.
- Crenshaw BS, Granger CB, Birnbaum Y, et al. Risk factors, angiographic patterns, and outcomes in patients with ventricular septal defect complicating acute myocardial infarction. GUSTO-I (global utilization of streptokinase and TPA for occluded coronary arteries) trial investigators. Circulation. 2000;101(1):27-32.