Question 4#
A 56-year-old male is diagnosed with a contained rupture of a thoracic aortic aneurysm and was emergently taken to the operating room for thoracic endovascular aortic repair. On postoperative day 1, he begins to complain of loss of motor function in his lower extremities. When reviewing the patient’s medication history, which of the following would place him at highest risk of developing a spinal hematoma after spinal drain placement?
A. Aspirin 81 mg taken the morning of surgeryB. Apixaban stopped 3 days before placement
C. Dabigatran stopped 4 days before placement
D. Enoxaparin DVT prophylaxis 14 hours before placement
Correct Answer is C
Comment:
Correct Answer: C
Consideration should be given with regard to preoperative placement of prophylactic lumbar spinal drain in patients at high risk for postoperative SCI; however, in patients who present for emergency repair of aortic aneurysm or dissection, a drain may not be placed because of time constraints. Postoperative rescue management of SCI includes therapies aimed at optimizing spinal cord perfusion pressure (the difference between the mean arterial pressure and either CSF pressure or central venous pressure, whichever is higher). This includes drainage of CSF via a subarachnoid drain, augmenting arterial pressure, and reducing central venous pressure or a combination of the three. The American Society of Regional Anesthesia and Pain Medicine (ASRA) published updated guidelines in 2018 for anticoagulation interruption before performing neuraxial techniques, which includes newer oral anticoagulation agents.
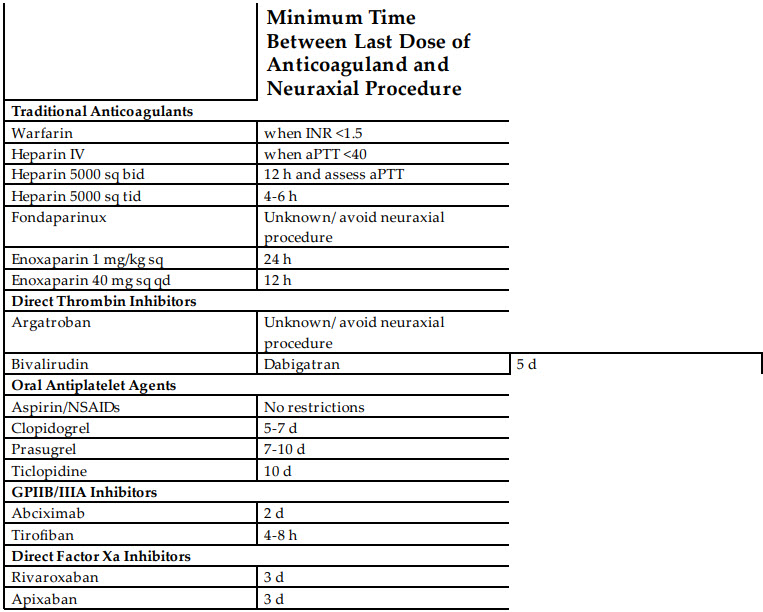
The table below includes recommendations from the most updated ASRA guidelines as of 2018.
In situations where the potential benefits outweigh the risks of neuraxial interventions such as lumbar spinal drain placement, clinical judgment as well as knowledge of the guidelines should be used.
Reference:
- Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy. Reg Anesth Pain Med. 2018;43(5):566.