Question 6#
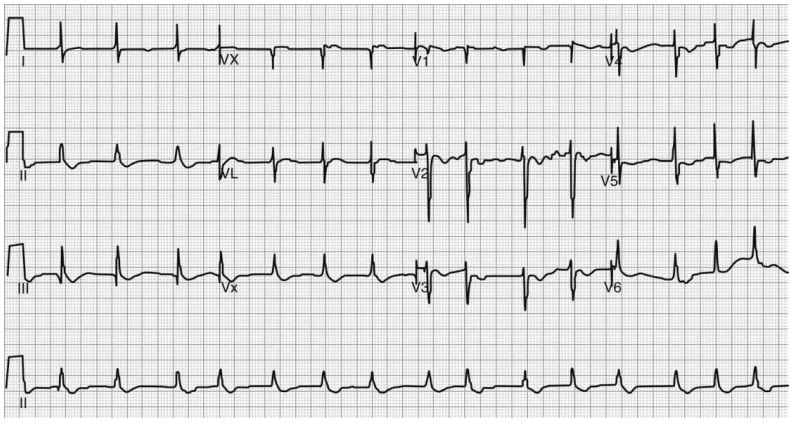
A 64-year-old male with a past medical history significant for hypertension, heart failure with reduced ejection fraction, myocardial infarction 2 years prior, and chronic kidney disease presents to the ICU following open AAA repair. He was restarted on his home medications on postoperative day 1. Three days later, his vitals and pertinent laboratory values include: blood pressure 150/100 mm Hg, heart rate 94 bpm, potassium 2.9 mmol/L, serum creatinine 2.6 mg/dL. The following electrocardiogram is obtained 24 hours after admission:
Which of the following medications was the patient most likely taking before surgery?
A. AtenololB. Digoxin
C. Lisinopril
D. Furosemide
Correct Answer is B
Comment:
Correct Answer: B
Digoxin is one of the oldest medications used to treat heart failure with reduced ejection fraction. Digoxin should be used with caution secondary to its narrow therapeutic window and significant risk of toxicity. Digoxin binds to the K+ site of the Na+/K+ adenosine triphosphate-ase pump and inhibits the ion transport, thus secondarily increasing intracellular calcium resulting in an ionotropic effect. Digoxin also has a stimulating effect on both sympathetic and parasympathetic tone with the latter being responsible for its chronotropic effects. Hypokalemia increases the risk of digoxin toxicity secondary to its interaction with the Na+/K+ ATPase pump. A number of other factors can also increase the risk of digoxin toxicity including hypomagnesaemia, hypercalcaemia, myocardial ischemia, hypoxemia, and acid-base disturbances. In addition, renal impairment can prolong the half life of digoxin, therefore increasing the risk of toxicity.
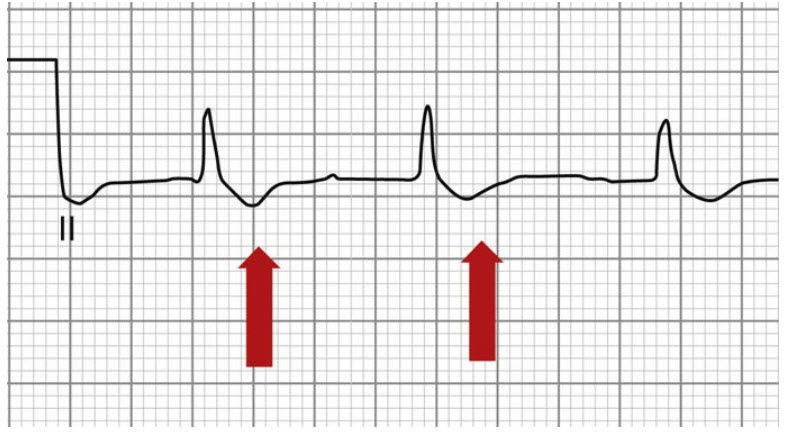
The electrocardiogram above shows characteristic ST segment downsloping depression as well as a shortened QT interval. However, a number of atrial and ventricular arrhythmias are possible with digoxin toxicity. Increased automaticity (atrial fibrillation/ flutter) with AV block, ventricular tachycardia, fibrillation and ectopy, and bradycardia can be seen.
Symptoms of acute digoxin toxicity include nausea, vomiting, diarrhea, hyperkalemia, lethargy, and confusion. The initial GI symptoms occur early at 2 to 4 hours post ingestion, with cardiovascular complications occuring later at 8 to 12 hours. Chronic digoxin toxicity typically has a more insidious onset and is often related to concurrent illness i.e. impaired renal function. The features are similar to acute toxicity with the addition of visual disturbances (reduced vision, yellow halos, and altered color perception) The treatment of digoxin toxicity is with Digoxin-specific Fab antibody fragments, which bind to molecules of digoxin, making them unavailable for binding at their site of action. Digoxin has a narrow therapeutic index and patients must be monitored closely to detect signs of toxicity in the setting of electrolyte, acid-base disturbances, and in renal impairment.
References:
- Bauman JL, DiDomenico RJ, Galanter WL. Mechanisms, manifestations, and management of digoxin toxicity in the modern era. Am J Cardiovasc Drugs. 2006;6(2):77-86. doi:10.2165/00129784-200606020-00002.
- Mladěnka P, Applová L, Patočka J, et al. Comprehensive review of cardiovascular toxicity of drugs and related agents. Med Res Rev. 2018;38(4):1332-1403. doi:10.1002/med.21476.