Question 8#
Which of the following potential complications IS NOT paired correctly with the corresponding classification of aortic dissection?
A. Elevated lactate, elevated INR and AKI—DeBakey Type IIB. Elevated troponin—Stanford Type A
C. New onset diastolic murmur heard at the right second intercostal space—DeBakey Type III
D. New onset right hemiplegia—DeBakey Type I
Correct Answer is A
Comment:
Correct Answer: A
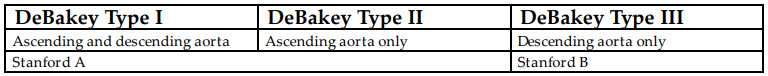
There are two main classification systems for thoracic aortic dissections, the Stanford classification and the DeBakey classification. Stanford Type A includes all dissections involving the ascending aorta regardless of the extent or site of origin. Stanford Type B includes all dissections distal from the left subclavian artery.
Stanford classification is focused on anticipated treatment of the dissection. Type A dissection accounts for about 60% of all dissections and mandates early surgical repair, as any delay carries a 2% increase in mortality for every hour delayed. Additionally, postponing repair increases the risk for developing life-threatening complications of proximal dissection, which include rupture into the pericardial sac with resulting cardiac tamponade, severe aortic regurgitation, and coronary artery occlusion from extension of the dissection flap into the coronary arteries with subsequent myocardial infarction. Type B dissections account for about 40% of aortic dissections and require medical management focused on decreasing the shear stress on the aortic wall, via reduction in both heart rate and arterial pressure. Surgical repair is indicated if there is severe compression of the true lumen or critical branches arising from the false lumen with signs of hypoperfusion to the lower extremities, visceral organs, and/ or kidneys.
The DeBakey classification takes into account the site of origin of the dissection and the extent of the dissection distally. Type I originated in the ascending aorta and propagates to the descending aorta. Type II originates within and is confined to the ascending aorta. Type III originates below the left subclavian artery and extends distally or, more rarely, retrogrades into the arch and ascending aorta.
By understanding these classification systems, the potential branch vessels that could be compromised by a dissection flap can be identified. Ischemic bowel is due to occlusion of visceral vessels branching off of the descending aorta and thus would not be affected in a DeBakey type II dissection, which is limited to the ascending aorta (A). Acute myocardial infarction can result from intimal flap dissection into a coronary artery. Cerebrovascular accident is a potential complication of dissections involving the carotid arteries. The aortic valve can also be compromised when a proximal dissection flap prolapses through the valve in diastole.
There is an uncommon form of aortic dissection, which originates as type III DeBakey, with subsequent retrograde (proximal) propagation to the aortic arch and ascending aorta. This scenario is not appropriately addressed by the DeBakey and Stanford classification systems. If the proximal propagation is confined within the aortic arch, then it is still considered type B. If the dissection involves the aorta proximal to the brachiocephalic trunk, then it is Stanford Type A.
There are two main systems for classifying aortic dissections; it is important to understand the dissection type as the complications vary. Beyond identifying branch vessels at risk of compromise based on dissection type, determining site of origin and propagation of the dissection is important as it effects management.
References:
- Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management. Circulation. 2003;108(6):772-778. doi:10.1161/01.cir.0000087400.48663.19.
- Emmett M. Predicting death in patients with acute type A aortic dissection. Circulation. 2002;106(25):e224. doi:10.1161/01.cir.0000043546.26296.d2.