Question 2#
A 68-year-old female with severe chronic obstructive pulmonary disease experienced a syncopal event while climbing the stairs at home. She presented to the emergency department with multiple rib and upper extremity fractures as well as a displaced hip fracture. Following an urgent hip fracture repair, she arrives to the ICU intubated and sedated. On physical examination, she has a laterally displaced point of maximal impulse with a systolic murmur heard best at the left sternal border.
Which transthoracic echocardiographic view would best aid in diagnosis and grading of severity?
A. Apical 4-chamberB. Suprasternal
C. Apical 3-chamber
D. Parasternal basal short axis
Correct Answer is C
Comment:
Correct Answer: C
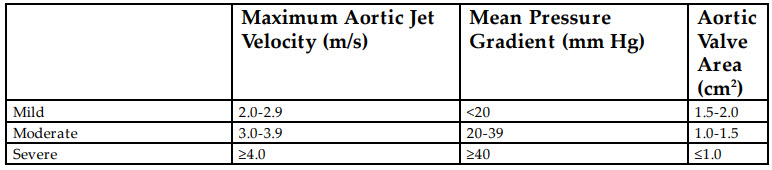
Given the physical examination findings, this patient likely has aortic stenosis. The degree of aortic stenosis is best evaluated in the apical 5- chamber and 3-chamber views. The apical 5-chamber view is obtained by tilting the probe anterior from the apical 4-chamber view until the left ventricular outflow tract and aortic valve come into view. The apical 3- chamber view is obtained rotating the probe counterclockwise at 60° from the apical 4-chamber view until the left atrium, left ventricle, left ventricular outflow tract, and aortic valve appear. Utilizing these views, continuous wave Doppler can be applied to obtain the velocity and gradient across the aortic valve. Valvular hemodynamic parameters classifying the degree of aortic stenosis are presented in the table below:
Aortic stenosis increases both the systolic and diastolic pressures of the left ventricle. Gradually increased systolic pressure leads to concentric left ventricular hypertrophy and myocardial remodeling. According to the Law of LaPlace (S = Pr/h; S = systolic wall stress, P = pressure, r = ventricular radius, and h = ventricular thickness), left ventricular hypertrophy results in increased wall thickness and therefore decreased wall stress. This hypertrophy can displace the point of maximal impulse laterally and may lead to the development of a fourth heart sound, S4 . Furthermore, the left ventricular ejection time is increased, which decreases the time spent in diastole. Increased left ventricular diastolic pressure combined with a decreased time in diastole will decrease coronary perfusion and promote myocardial ischemia.
The definitive management of patients with aortic stenosis is aortic valve replacement. ICU management focuses on the following hemodynamic goals: correction of hypovolemia (decreased preload), avoidance of tachycardia, normal but not augmented inotropy and aggressive treatment of hypotension (maintaining afterload). Maintaining left ventricular filling pressure is vital to promote ejection in the setting of high transvalvular gradients. Reduced afterload should be aggressively treated and counteracted to increase diastolic blood pressure and restore coronary perfusion pressure. It is also important to avoid increases in myocardial oxygen demand such as pain, tachycardia, and other increases in sympathetic drive. In summary, the main hemodynamic goals in patients with severe aortic stenosis are to maintain adequate preload, increase afterload, avoid tachycardia, and maintain normal contractility.
References:
- Lindman BR, Clavel MA, Mathieu P, et al. Calcific aortic stenosis. Nat Rev Dis Primers. 2016;2:16006.
- Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the european association of cardiovascular imaging and the american society of echocardiography. J Am Soc Echocardiogr. 2017;30:372-392.