Question 4#
A 75-year-old male is brought to the Emergency Department with severe hypotension. He has a past medical history of heart failure with reduced ejection fraction (last EF 24%) and has not been compliant with his diuretics or diet. He has been admitted multiple times in the past year for heart failure exacerbations. On arrival to the Emergency Department, he is cool and minimally responsive with an initial blood bilateral pressure of 70/40 mm Hg. He is started on dobutamine and norepinephrine. On arrival to the ICU, the patient has a right radial arterial line placed without complication. The monitor reports a blood pressure of 65/55 mm Hg. The blood pressure is immediately rechecked manually, and a reading of 80/40 mm Hg is obtained.
Which of the following is the MOST likely reason for this discrepancy?
A. Failure to adequately prime arterial lineB. Patient has severe aortic regurgitation
C. Patient has severe peripheral vascular disease
D. Patient has concurrent sepsis
Correct Answer is A
Comment:
Correct Answer: A
Arterial lines are useful to receive quick and real-time information about a patient’s hemodynamics. An arterial line has a catheter (inserted into the patient) that transmits the pressure wave to the fluid-filled tubes of the monitoring system. The tubing system carries the impulse of the pressure wave to the transducer, which converts the mechanical pressure signal to an electrical signal that is then presented on the monitor as a waveform. There are three steps in the calibration of an arterial pressure line:
- Priming—the air is removed out of the pressure tubing system
- Leveling—the pressure transducer is kept at the level of the heart to most accurately capture the mean arterial pressure/aortic pressure without further effects of gravity
- Zeroing—the pressure transducer is calibrated to atmospheric pressure as the zero point to better allow for interpretation of the arterial line blood pressures
If the arterial line system is not primed, an air bubble is introduced into what should be a fluid-filled tubing system. Air dampens pressure signals more than fluid does, so if an air bubble is introduced into the system, the waveform amplitude reflects serious dampening and reads systolic pressures as lower than actual and diastolic pressures higher than actual.
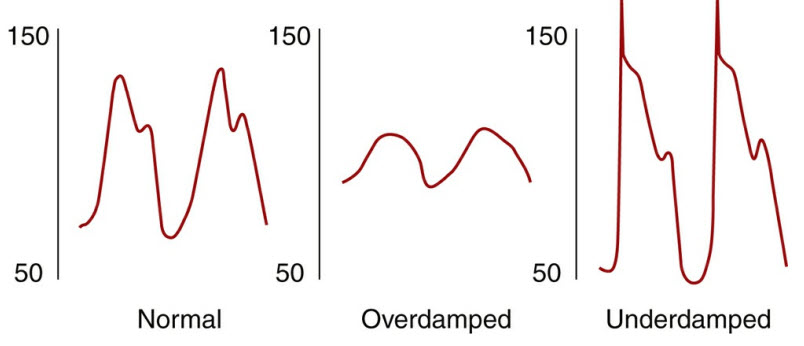
Underdamping can be caused by aortic regurgitation or hyperdynamic states such as sepsis (that would cause a widened pulse pressure). Disappearance of the diastolic waveform can be seen in patients with significant peripheral vascular disease.
References:
- Barash PG, Cullen BF, Stoelting RK, et al. Clinical anesthesia. Chapter 25: Commonly Used Monitoring Techniques. Philadelphia: Lippincott, Williams & Wilkins; 2013.
- https://www.aic.cuhk.edu.hk/web8/haemodynamic%20monitoring%20