Question 5#
A 54-year-old man with a history of moderate COPD is transferred from the floor to the ICU one day after a witnessed aspiration event for increased work of breathing. On examination, pulmonary auscultation reveals bilateral rhonchi but no wheezing, and chest radiograph shows new bilateral, patchy pulmonary opacities. Respiratory rate is 36, and the patient communicates in one to three word sentences between breaths. Initial arterial blood gas analysis shows:
- pH 7.34
- PaCO2 65
- PaO2 135 on 15L non-rebreather face mask
What is the next best step?
A. Trial of noninvasive ventilation (NIV)B. Ipratropium/albuterol nebulizer
C. Intubation and mechanical ventilation
D. Furosemide IV bolus
Correct Answer is C
Comment:
Correct Answer: C
The patient meets criteria for ARDS, although severity stratification based on the Berlin criteria requires PEEP >5 cm H2O.
The Berlin Criteria for Acute Respiratory Distress Syndrome:
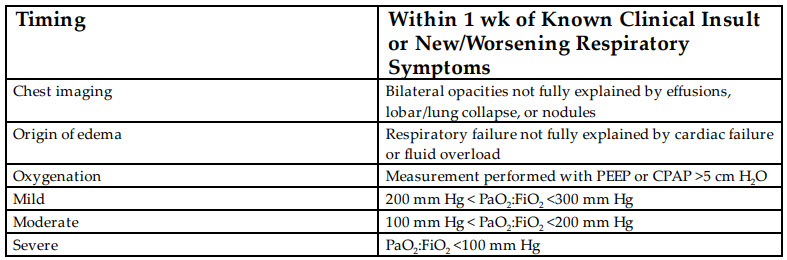
Given the signs of increased work of breathing, with difficulty managing full sentences on face mask, an ABG demonstrating an uncompensated acute-on-chronic respiratory acidosis indicating progressive CO2 retention, and persistent hypoxemia on non-rebreather, the patient should be intubated and receive mechanical ventilation with low tidal volumes (4- 6 mL/kg), plateau pressure <30 cm H2O, and PEEP >5 cm H2O.
NIV can be used as an initial ventilatory support in patients with acute respiratory failure to spare the risks associated with sedation, muscular paralysis, and ventilator-associated complications. Several concerns remain regarding its use in the ARDS population, and the subgroups of ARDS most likely to benefit from it remain unclear. In particular, the use of prolonged NIV in the absence of respiratory function improvement may delay intubation and mechanical ventilation in patients who would benefit from conventional ARDS ventilation strategies. Recent data suggest that increased ARDS severity based on PaO2 :FiO2 was associated with NIV failure, and that NIV used was associated with increased ICU (although not hospital) mortality. In particular, NIV use was associated with higher ICU mortality in patients with PaO2 :FiO2 <150 mm Hg. NIV use may best be reserved for patients with mild ARDS (PaO2 :FiO2 201-300 mm Hg.) Other contraindications to NIV use include inability to cooperate because of altered mental status, inability to protect the airway or clear secretions, recent facial surgery or trauma, and recent esophageal anastomosis.
This patient with COPD may benefit from an ipratropium/albuterol nebulizer, but given adequate air excursion and the absence of wheezing, bronchospasm is likely not the central pathophysiology driving his clinical decompensation. Similarly, furosemide bolus is unlikely to significantly improve his ventilation in the absence of signs of volume overload.
References:
- Bellani G, Laffey J, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE Study. Am J Respir Crit Care Med. 2017;195(1):67-77.
- Rana S, Jenad H, Gay PC, Buck CF, Hubmayr RD, Gajic O. Failure of noninvasive ventilation in patients with acute lung injury: observational cohort study. Crit Care. 2006;10:R79.
- Chawla R, Mansuriya J, Modi N, Pandey A, Juneja D, Chawla A, Kansal S. Acute respiratory distress syndrome: predictors of noninvasive ventilation failure and intensive care unit mortality in clinical practice. J Crit Care. 2016;31:26-30.
- Ranieri VM, Rubenfeld GD, Thompson BT, et al; ARDS Definition Task Force. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526-2533.