Question 11#
An 89-year-old bedridden man with a history of dementia, non– insulin-dependent diabetes, hip fracture (treated conservatively), diastolic heart failure, and chronic kidney disease was admitted to the medicine service for confusion and possible UTI. The patient had a one week hospital admission for UTI one month ago. While he was waiting for bed assignment, he starts to desaturate in the emergency department. His vital signs are heart rate 115 beats/min, blood pressure 100/60 mm Hg, respiratory rate 26 breaths/min, SpO2 86% on room air. Lung auscultation was unrevealing. You were consulted by the medicine team to evaluate the patient for possible ICU admission for hypoxic repository failure. Portable x-ray was negative for any acute process per radiology official read. Your bedside lung ultrasound images show the following:
Besides placing the patient on oxygen, what would be the BEST next step in management?
A. Start the patient on antibiotics hospital acquire pneumoniaB. Order a STAT CT angiogram of the chest to rule out pulmonary embolism
C. Order furosemide to treat pulmonary edema
D. Place chest tube to treat pleural effusion
Correct Answer is A
Comment:
Correct Answer: A
Based on the ultrasound images, this patient likely has pneumonia (answer A). The negative auscultation findings and negative chest x-ray cannot rule out pneumonia due to their low accuracy and negative predictive values. Moreover, chest x-ray diagnostic accuracy for pneumonia has been questioned. Bourcier et al. showed that chest x-ray has low sensitivity in diagnosing pneumonia when compared to lung ultrasound (95 vs. 60%).
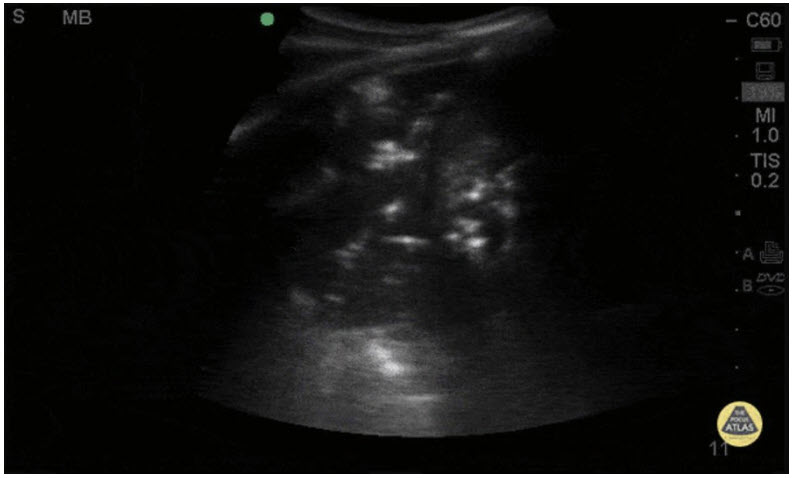
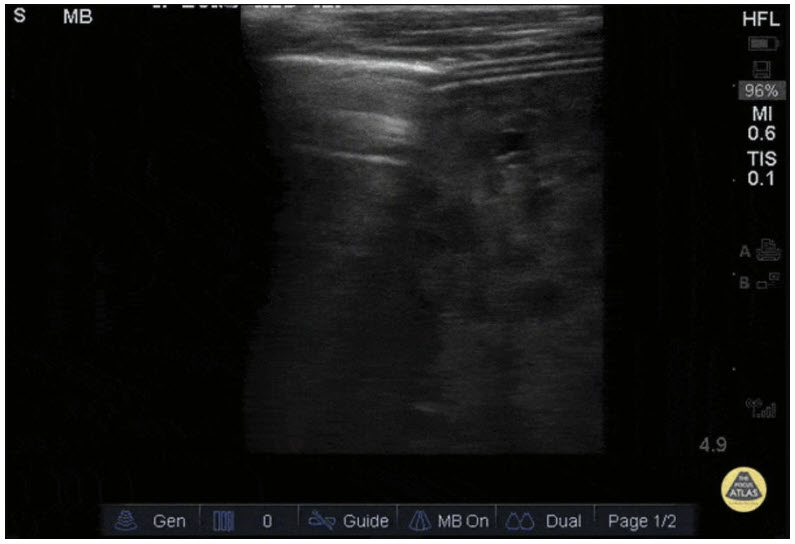
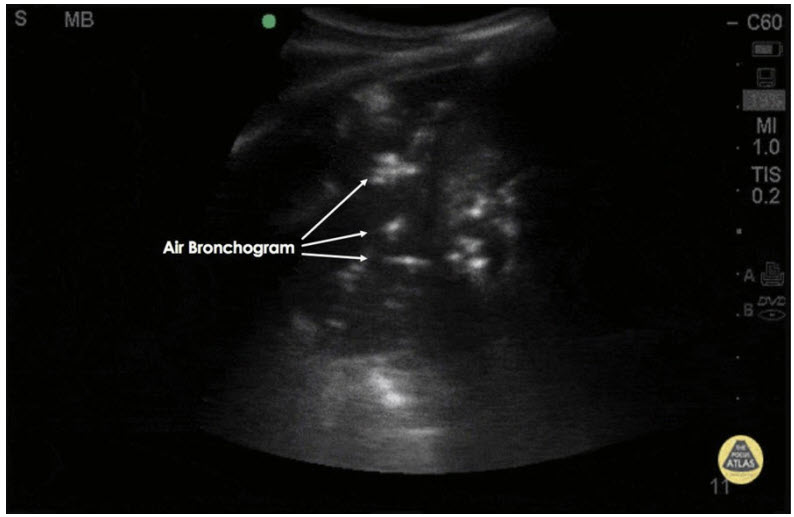
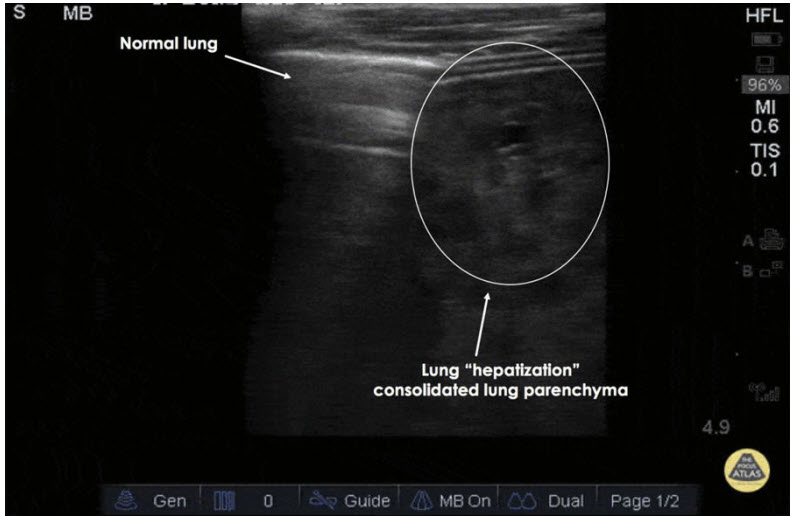
Multiple sonographic signs were described in the literature to assist in the diagnosis of pneumonia. These signs include b-lines, air bronchograms, subpleural consolidations “hepatization,” pleural line abnormalities, and pleural effusions. Air bronchograms and subpleural consolidations “hepatization” are the most specific sonographic signs. Air bronchograms are thought to be caused by air trapped in small airways within a consolidated lung. On ultrasound, it will look like hyperechoic dots and lines (air) within a hypoechoic (fluid) area (Figure 1). Subpleural consolidations, which also known as “hepatization,” is a sonographic sign of consolidated lung. Typically, the lung parenchyma is not visible on ultrasound since air does not conduct sound waves, but when small airways and alveoli get filled by purulent fluid, sound waves will be able to go through the lung parenchyma. Sonographically, consolidated lungs will have the echotexture of the liver, hence the name hepatization of lungs.
Answers C and D are both incorrect because the patient does not have sonographic signs suggesting pleural edema or effusion. Pulmonary embolism can cause peripheral lung parenchyma infarction, which sonographically appears like consolidation. The presence of air bronchograms, on the other hand, is pathognomonic of pneumonia.
References:
- Metlay JP, Kapoor WN, Fine MJ. Does this patient have communityacquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-1445.
- Bourcier JE, Paquet J, Seinger M, et al. Performance comparison of lung ultrasound and chest x-ray for the diagnosis of pneumonia in the ED. Am J Emerg Med. 2014;32(2):115-118.
- Ticinesi A, Lauretani F, Nouvenne A, et al. Lung ultrasound and chest xray for detecting pneumonia in an acute geriatric ward. Medicine. 2016;95:e4153.
- Blaivas M. Lung ultrasound in evaluation of pneumonia. J Ultrasound Med. 2012;31(6):823-826.
- The POCUS Atlas. Available at http://www.thepocusatlas.com/pulmonary1/ohidf6dvg076d2jzmel6c733cs2y5w. Accessed November 1, 2018.
- The POCUS Atlas. Available at http://www.thepocusatlas.com/pulmonary1/7z96r1evhnr2eyjwagn2e8o8jacqbh. Accessed November 1, 2018.