Question 4#
A 32-year-old male is referred to the nephrologist for abnormal laboratory values. He was recently seen by his primary care physician for his annual physical examination. During his visit, he was told that his “urine was abnormal.” The patient does not have any known medical history except for a 26-year pack-year smoking history. He is normothermic with a blood pressure of 128/90 mm Hg, pulse rate of 58 beats/min, and respiratory rate of 12 breaths/min. The rest of his physical examination is unremarkable. His family history is only significant for arthritis and “thyroid disease.” Further laboratory studies obtained show the following:
- Sodium 142 mEq/L (mmol/L)
- Potassium 3.3 mEq/L (mmol/L)
- Chloride 117 mEq/L (mmol/L)
- Bicarbonate 10 mEq/L (mmol/L)
- Glucose 243 mg/dL
- BUN 22 mg/dL
- Creatinine 1.3 mg/dL (baseline is 1.1)
- Albumin 4.2 g/L
- Urine pH 5.6
- Urine sodium 62 mEq/L
- Urine potassium 85mEq/L
- Urine chloride 126 mEq/L
- Urine calcium 378 mg/dL
What is the MOST likely diagnosis in this patient?
A. Gitelman syndromeB. Renal tubular acidosis (RTA) type 1
C. RTA type 2
D. Bartter syndrome
E. Salicylate toxicity
Correct Answer is B
Comment:
Correct Answer: B
This patient likely has RTA type 1. In patients with RTA type 1, there is impairment of acidification in the distal part of the nephrons. Because the kidney is unable to excrete hydrogen ions, this defect leads to the secretion of NH4+ . Patients with RTA type 1 usually have non–anion gap acidosis (which is also found in patients with RTA type 2 and 4). However, the main difference between the types of RTA is that type 1 will also have very low levels of HCO3 − , high urine pH of >5.5 (as the kidney is unable to maximally acidify the urine), and positive urine anion gap. In this case, the patient’s urine anion gap is 19 based on the formula, Urine anion gap = UNa + UK − UCl .
Main causes of RTA type I include autoimmune diseases, such as rheumatoid arthritis and Sjögren syndrome, obstructive nephropathy, and nephrotoxins, including toluene and amphotericin B. There is a hereditary cause for RTA type 1 which is usually diagnosed in infants or childhood. Though the clear mechanism of acquired RTA type I is unclear, it has been suggested that this due to defective H+ -K+ ATPase function at the apical surface of the α-type intercalated cells of the collecting duct.
In children, this can manifest with polyuria, stunted growth, recurrent nephrocalcinosis, and hypercalciuria. In adults, RTA type 1 will also lead to nephrocalcinosis. Treatment consists of managing the underlying disorders but can sometimes include usage of thiazide diuretics and/or NaHCO3 and K+ supplementation.
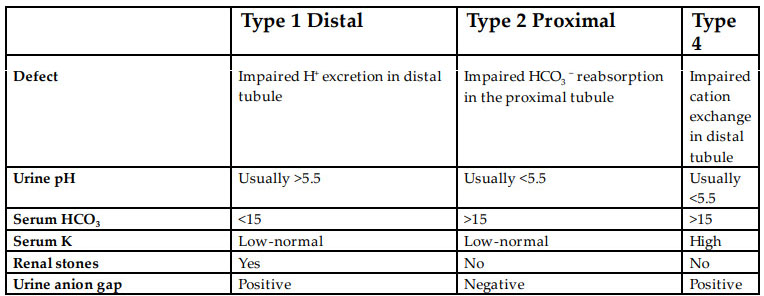
While all types of RTA lead to hyperchloremic non–anion gap metabolic acidosis, the main differences between types of RTA are laid out in the table below:
Reference:
- Soriano JG. Renal tubular acidosis: the clinical entity. J Am Soc Nephrol. 2002;13:2160-2170.