Question 5#
A 66-year-old man is brought to the ED with a 3-week history of generalized malaise and worsening right-sided headaches not responding to acetaminophen or ibuprofen. He has a past medical history significant for hypertension, hyperlipidemia, moderate obesity, and recurrent otitis media and had an episode of pneumonia about 4 years ago. He is awake, alert, and well-oriented. Vital signs are within normal limits. Heart and lung sounds are normal, abdomen is soft and nontender, and neurological examination including cranial nerves is normal and symmetrical. Complete blood count and metabolic panel are within normal limits except for a mild leukocytosis and mild hyponatremia. Erythrocyte sedimentation rate (ESR) is 62 mm/h and a nasal swab for methicillin-resistant Staphylococcus aureus is negative by PCR. A CT of the head without contrast shows a single 2 cm lesion in the right temporal lobe with mild surrounding edema, which the radiologist reports as concerning for an abscess. Also seen are some microvascular ischemic changes and opacification of right mastoid air cells. The patient is started on vancomycin and piperacillin/tazobactam and transferred to the neurological ICU for further management.
Which of the following changes to the antibiotic regimen is MOST appropriate for this patient
A. Continue vancomycin and piperacillin/tazobactam. Start voriconazoleB. Continue vancomycin. Stop Piperacillin/Tazobactam. Start Cefriaxone and Metronidazole
C. Continue Vancomycin. Stop piperacillin/tazobactam. Start ceftriaxone, metronidazole, and amphotericin B
D. Stop vancomycin and piperacillin/tazobactam. Start ceftriaxone and metronidazole
Correct Answer is D
Comment:
Correct Answer: D
This patient has a temporal lobe abscess associated with recurrent otitis media infection and mastoiditis. He does not have a history of transplantation or immunocompromise, and MRSA PCR is negative. Consequently there is no need of antimicrobial coverage for methicillinresistant Staphylococcus aureus (MRSA), atypical bacteria, fungi, or parasites. He should be empirically treated with a third-generation cephalosporin and metronidazole.
Although cryptogenic brain abscesses do occur, most focal brain parenchymal infections are associated with either a contiguous focus of infection (dental infection, otitis media, mastoiditis, sinusitis, meningitis), introduced directly by disruption of physical barriers in the area (recent dental or neurological procedure, head trauma), or via hematogenous spread from distant source (endocarditis, lung infection). When the source is adjacent, there is usually only a solitary abscess, whereas multiple abscesses are commonly seen with hematogenous spread from more distant sources. The location of the abscess also can provide some clues to the etiology. The causative organisms in these cases are typically the ones causing the primary infection. However, underlying host characteristics can predispose to brain abscesses by unusual or atypical bacteria, parasites, and/or fungi, for example in patients with HIV, solid organ transplant (SOT), hematopoietic stem cell transplant (HSCT), neutropenia, other forms of immunosuppression, or in those with diabetes and cyanotic heart disease (see table). The source of infection and the predisposing factors should therefore be taken into consideration while designing an empiric antimicrobial regimen.
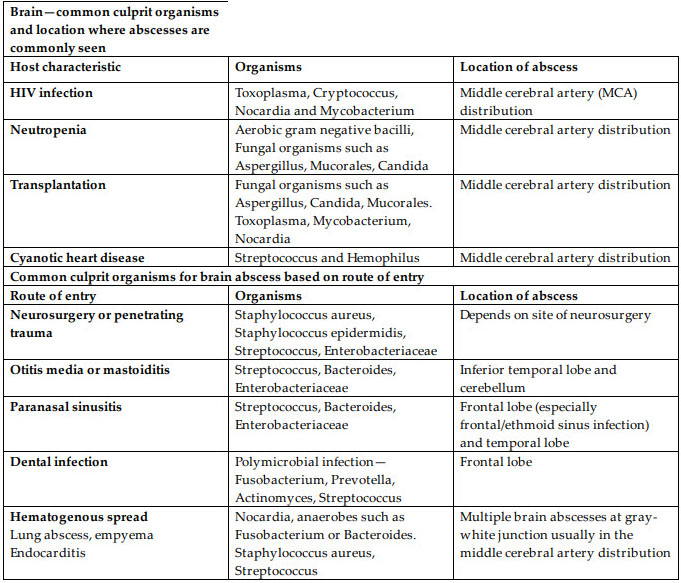
Based on the principles discussed above, the empiric antibiotic therapy for suspected brain abscess can be summarized as:
- Empiric coverage in an immunocompetent patient with a suspected or confirmed contiguous route of entry of infection such as otitis media/mastoiditis or paranasal sinusitis is a combination of third-generation cephalosporin (eg ceftriaxone) plus metronidazole for anaerobic coverage.
- In cryptogenic cases where there is no identifiable source and MRSA is a potential pathogen, vancomycin should be added to the basic empiric regimen of third-generation cephalosporin plus metronidazole.
- In the setting of prior neurosurgical intervention or in trauma, an antipseudomonal cephalosporin (eg cefepime or ceftazidime) should be used in combinmation with vancomycin to cover for healthcare associated MRSA.
- In HIV-infected patients, empiric coverage for toxoplasmosis, Cryptococcus, and Nocardia should be considered depending on the clinical scenario. Therapy for tuberculosis is reserved for confirmed cases or in whom other diagnoses have been reasonably excluded and, in general, should not be started as part of an empiric regimen.
- For SOT and HSCT recipients, empiric coverage for toxoplasmosis and Nocardia should be considered as well as empiric fungal coverage for Candida and/or Aspergillus.
References:
- Brouwer MC, Coutinho JM, van de Beek D, Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014;82:806-813.
- Brouwer MC, Tunkel AR, McKhann GM II, van de Beek D. Brain abscess. N Engl Med. 2014;371:447-456.
- Brook I. Microbiology and treatment of brain abscess. J Clin Neurosci. 2017;38:8-12.