Question 4#
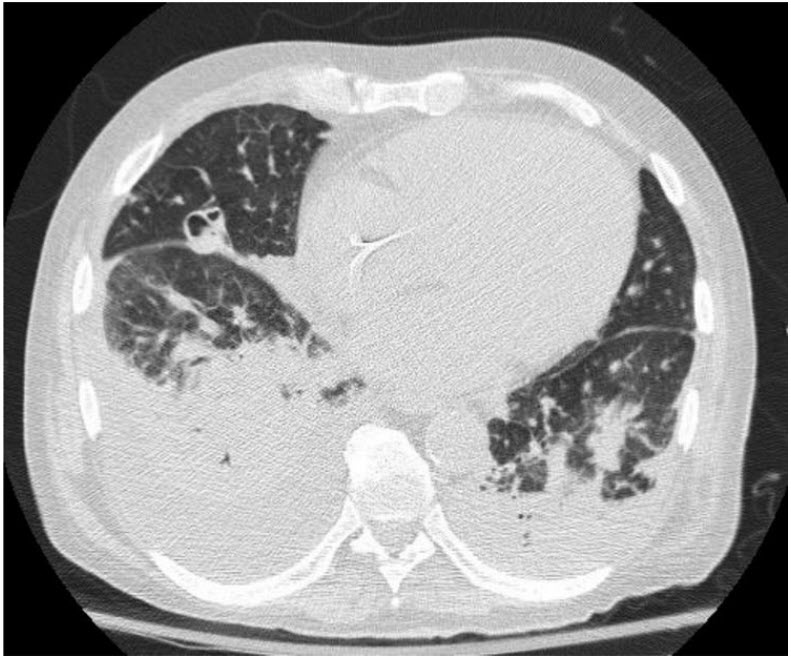
A 58-year-old man with a new diagnosis of AML receives induction chemotherapy with cytarabine and doxorubicin on the Oncology ward. About 10 days later he develops neutropenic fever in association with worsening hypoxemic respiratory failure. A chest CT is performed (see figure below) and Infectious Disease and Pulmonary are consulted, with bronchoscopy performed the following day notable for friable-appearing airways but with minimal mucous. Gram stain of BAL is unrevealing. Postbronchoscopy the patient has worsening hypoxemic respiratory failure and is transferred to the ICU and intubated. Despite the administration of vancomycin, cefepime, and voriconazole, fevers persist and hypoxemia continues to worsen, requiring high levels of ventilator support. Serial plain films of the chest show progressive whiteout on the right side. Three days postintubation the patient develops massive hemoptysis and cannot be ventilated, resulting in cardiac arrest and subsequent transition to comfort measures after discussion with family.
The BAL cultures are most likely to show:
A. Staphylococcus aureusB. Streptococcus pneumoniae
C. Pseudomonas aeruginosa
D. Aspergillus fumigatus
E. Influenza A
Correct Answer is D
Comment:
Correct Answer: D
The chest CT reveals a cavitary nodule, which in neutropenic patients (severely immunocompromised as in this patient who recently received cytotoxic chemotherapy) is highly concerning for a fungal infection. Although lung cavitation may be seen with bacterial infection (especially Staph, Klebsiella, Nocardia, and occasionally Pseudomonas), with such a high burden of disease Gram stain is likely to be positive and the patient would likely be producing more airway secretions than described (though notably with systemic neutropenia secretions are less purulent than in an immunocompetent host.) A. fumigatus is a ubiquitous mold that causes a spectrum of disease ranging from allergic airway disease to IPA as in this case. KOH stains of respiratory secretions may reveal fungal elements; however, identification of the species requires sporulation and typically takes several days. Galactomannan is a component of Aspergillus (and other mold) cell walls and may be tested in blood and BAL. While awaiting the definitive diagnosis of species and susceptibility, some experts recommend broadening from voriconazole to liposomal amphotericin; though with the introduction of the newer antifungal azoles posaconazole and isavuconazole, this decision should involve expert consultation. Regardless of the mold drug sensitivities, drug penetration into areas of lung destruction by angioinvasive molds is poor and mortality is very high. Notably, lung resection in cases of invasive mold disease in bone marrow transplant patients has been described.
Reference:
- Bernard A, Caillot D, Couaillier JF, et al. Surgical management of invasive pulmonary aspergillosis in neutropenic patients. Ann Thorac Surg. 1997;64:1441-1447.